'My biggest fear is if I get infected will I get admission in a good hospital and how much money will the hospital charge for my treatment.'

Jitendra Laxman Shelatkar, 46, has been an ambulance operator since 1998.
With a huge EMI burden on his shoulders and without much work since the lockdown began, Jitendra began ferrying COVID-19 positive patients only from the last week of May, as non-COVID patients had dried up in the face of hospitals refusing admissions to them.
"One feels excruciatingly hot once inside the PPE kit leading to loss of water from our bodies. That would sometimes lead to suffocation, breathing issues, regular thirstiness, skin irritation, dizziness and nausea," Jitendra Shelatkar tells Prasanna D Zore/Rediff.com in our continuing series on COVID-19 Warriors.
While I started my journey as an ambulance operator in 1998, it was only in 2002-2003 that I began to see the scary side of it. It was then that I began taking AIDS patients to hospitals.
At that time precautions meant using only masks and gloves. There were no sanitisers or personal protection equipment (PPE) kits then.
Doctors would often advise us to take care as there was not much awareness about how the AIDS virus infected people and there were lot of misconceptions too.
There was more fear and less awareness about how a person got infected by AIDS and so there were insecurities and fears.
More than the fear of contracting AIDS the social stigma linked to AIDS was scarier.
There were also risks associated with carrying patients suffering from Open Cox, a type of TB, to hospitals.
I have been ferrying COVID-19 patients since the last week of May.
In the beginning, I had no idea about PPE kits, sanitisers, etc. Private ambulance operators had no guidelines issued by the BMC (BrihanMumbai Municipal Corporation) or the state health ministry if we could ferry COVID-19 patients.
If a person tested positive for COVID, the pathological lab/doctors would contact the BMC, which in turn would contact 108 and take COVID positive patients to hospitals.
Later, as the number of cases began ballooning, private ambulances were roped in.
I took my first positive patient from a private hospital in Malad East to a nursing home in Malad West (both in north west Mumbai).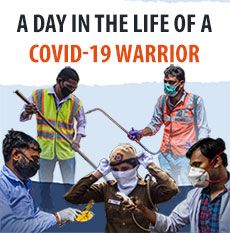
This patient was serious but had recovered completely. Since he could not cope with the huge medical expenses, which were around Rs 18,000 per day at this hospital, the doctors there suggested that he move to some other hospital and quarantine himself for the remaining period of recovery.
Since then, I have been taking at least one COVID-19 patient per week to various hospitals for treatment.
The challenges
There was this positive patient suffering from Alzheimer's who would not do what we asked him to do while being shifted to the hospital. He, perhaps, was unable to understand what we were telling him.
Despite several efforts he would not walk on his own to the ambulance. Left with no choice we -- my assistant and I -- had no choice but to haul him up on my shoulder into the ambulance.
We have been taught by medical professionals on how to don and doff the PPE kit.
Driving the ambulance with the entire PPE kit is a big task. At least, for the first few days till we began to acclimatise ourselves to wearing PPE kits for several hours -- from the time we took the patients from their homes and got them admitted into hospitals.
One feels excruciatingly hot once inside the PPE kit -- especially in May and June -- leading to loss of water from our bodies. That would sometimes lead to suffocation, breathing issues, regular thirstiness, skin irritation, dizziness and nausea.
Even if we have to wear it for not more than two hours generally, it becomes unbearable.
I had purple patches all over my skin for the first few times I donned the PPE. I had to take medicines to take care of it.
We purchase the PPE kit on our own and then bill the patient for it. In the beginning as I bought few pieces I had to shell out Rs 2,400 per PPE kit. Then I purchased 20 PPE kits in bulk and had the price reduced to Rs 1,600. I still have four left with me.
Carrying patients on the stretcher as well as walking is a task after wearing the PPE kit. We charge Rs 4,000 per patient.
The state government has taken a good decision to cap the prices that ambulance operators can charge. I have seen patients and their families being looted by some operators who charge even Rs 25,000 to carry COVID-19 patients to the hospital. The government should have acted much before this.
For the first few calls, we were called by hospital doctors to get COVID positive patients from their homes to the hospitals. Now, we get direct calls from the relatives of the patients or from the BMC about the details of the patient who needs to be taken to the hospital.
While some patients are fit enough to walk on their own into the ambulance there are times we have to stretcher them, or as I told you earlier haul them to the vehicle.
The very first experience
When I reached the hospital to shift this patient I was asked to wait for some time as the discharge formalities were under process.
The patient's son called us around 10 am to reach the hospital by 10.30 am all geared in PPE suits. When we reached there a few minutes before 10.30, the patient's son was busy with discharge formalities.
He would come out every 15 minutes and ask me to wait for another 15 minutes. This continued for almost three hours before the patient was finally discharged by 1.30 pm.
My assistant and I had to remain inside the PPE kit for almost four hours, including the time by when we got him admitted to the other hospital.
And the next one...
There was this patient in Goregaon (north west Mumbai) whose relative called us for our services. The patient, an 80-year-old lady, though not suffering from COVID, was quite critical and needed oxygen support, which is available in my ambulance.
I wasn't donning the PPE kit at that time because the patient's relative had assured us that his mother was not COVID positive.
We first took her to a hospital in Kandivali (north west Mumbai) because the patient's kin knew some doctor in that hospital. When the doctors checked that her oxygen saturation level had dropped to 65 they advised the relative to take her to some other hospital.
From there we took her to another nearby hospital which also refused admission saying they did not have adequate equipment to deal with the lady's situation.
At the next hospital, the hospital's nursing staff scanned her chest with an X-ray and they said the lady could be a suspected COVID-19 patient.
They also refused admission to her.
From there we went to two more hospitals in Malad, which too refused to admit her.
The family was about to take her back home when her daughter objected to bringing a suspected COVID-19 patient home. She had some contacts at an Andheri East hospital (north west Mumbai) and so she asked us to take her mother there. They too refused her admission.
From there we took her to another hospital in Andheri West. When they too refused to take her, we took her to a big hospital in Versova. They too did not budge despite desperate pleas from the lady's son.
Despite the lady being very serious none of the hospitals allowed the ambulance to enter their hospital premises. At all the hospitals, we were asked to move from the main gate.
All the hospitals said they did not have beds to treat or admit non-COVID patients and since she had not done her test they would not admit her.
From there we moved her to yet another private hospital in Vile Parle (north west Mumbai) and then again, when they did not take her, we took her to a nearby municipal hospital.
While we were allowed inside the premises of this municipal hospital and they showed signs of admitting her but only if we took her along with my ambulance's oxygen cylinder; they said they did not have enough oxygen cylinders in the hospital.
We were made to wait there for almost 90 minutes after which they refused admission because they did not have enough oxygen cylinders.
We were trying to get her admitted to a hospital around 9.30 pm the previous night and till 6 am the next day we kept running from hospital-to-hospital without any success.
By then my oxygen cylinder had almost emptied out so we called for a cylinder from the first hospital in Kandivali where we had taken her the previous night.
This cylinder was taken to her home in Goregaon where we took this lady after more than eight harrowing hours as the family, now completely fed up and drained of energies, decided to take her home and treat her there.
Two days later, the lady passed away.
And yet one more...

One day I got a call at around 1 pm from a patient's relative, a girl I know from Panvel (a township on the outskirts of Mumbai), who was not with the COVID patient.
She requested me to take her father from Goregaon to a big BMC-run hospital in Mumbai Central and said that one of his relatives would accompany the patient.
The patient and his son, who was with him, were from Uttar Pradesh and since they were new to the city were completely lost about the admission procedure at this hospital.
The patient's son could neither read nor write and so could not fill the various forms that had to be filled for his father's admission.
The daughter informed me that I had to take him to this hospital and contact a doctor she knew there who would help with the admission process.
I completed all the formalities beginning from his admission process to the time he was shifted to a ward all the while wearing the PPE suit.
That day I donned the PPE kit around 12.45 pm and remained in it till about 6 pm when the admission process was completed.
Once we reached the hospital's casualty ward, the staff was quite rude. Thankfully, one of the other patient's relatives asked us to take him to a ward where they checked the fever of incoming patients.
Since the doctors and medical staff were attending other patients this man, who had breathing problems and was using oxygen, had to wait for his turn.
Once we took him inside this fever clinic they checked his temperature, oxygen saturation and other vital parameters and after filling some forms, which I had to fill, they asked us to take the patient to room 3 or 4 but did not pinpoint the exact location where these rooms were.
After we reached room 3, which was at the far end from the fever clinic, they too conducted some tests and asked us to proceed to room 4 for the registration process.
After registration, they asked us to take the patient to ward no. 3 on the sixth floor.
As luck would have it, this was a female patient ward. When we came across a medical staff, who was wearing a PPE kit, she told us to take him to another room and find any vacant bed and out him up there.
We did find a vacant bed, but it was not properly done. When we told the staff there about it they sent for help which arrived 30 minutes later and then we finally got him admitted.
They asked us to keep the patient's clothes separately for which we had no carry bag. So, I went downstairs and brought one.
Personal fears
There have been instances when the patient was not tested for COVID-19, and so was apparently negative, but turned positive two days later when tests were done.
At such times, if the patient is not positive we don't wear PPE suits or face shields or other protective gear to avoid getting infected.
Ever since I began ferrying positive patients to hospitals there is a constant fear about getting infected.
In the beginning when there was not much awareness I have no idea how many positive patients I may have taken to hospitals unknowingly. But I would carry on a few days later if I didn't show any symptoms.
While that fear always remain hidden somewhere inside me that I too can get infected, I now know that the death rate is not too high and a healthy person like me has a higher probability of getting cured even if I am infected gives some hope and dispels some fears.
My biggest fear is if I get infected will I get admission in a good hospital and how much money will the hospital charge for my treatment.
If I get infected, how will I manage a minimum of Rs 6 lakh to Rs 7 lakh, or, maximum of Rs 13 lakh to Rs 14 lakh, that I hear from many people is the average cost of treatment of COVID-19 at small and big private hospitals.
I have to pay EMIs worth Rs 80,000 for a gold loan and home loan I have taken and since the last three months there isn't enough income because hospitals are not treating non-COVID patients.
If I get infected, all my dreams for myself and my family will be ruined.
I definitely don't feel like a warrior fighting some unknown disease, but it really feels good to see smiles on the faces of relatives as well as COVID-19 positive patients when they get admitted to a hospital when they most need it.
Disposing off the PPE kits
We sanitise ourselves as well as the PPE kit before donning it using sprays. We wear just one glove first; then cap, goggle, mask, shoes, face shield and then don the entire PPE suit.
When we go to the patient's house we wear the second pair of gloves.
While doffing the PPE kit we spray ourselves with sanitiser and remove the gloves in the end.
We make sure to wear two sets of gloves and two masks.
While removing the outer pair of gloves, we do not touch the outer surface that had come in contact with a positive patient.
We roll and fold the gloves to ensure that we don't touch the outer surface.
Then we remove the face shield first; then the entire suit; then shoes, cap and goggles.
We dispose off the entire PPE suit, the pair of outer gloves, and the outer face mask properly inside a designated bin at the hospital where the patient is admitted.
Every hospital has the facility for disposing off the PPE kit.
Once we reach home, we sanitise ourselves, our gloves and mask again and then dispose off the inner pair of gloves and face mask in a bin after carefully tucking it inside a plastic bag.
We take a hot water bath and also wash our clothes using hot water.










 © 2025
© 2025