'We started analysing young patients and realised that they had causes like undetected diabetes, which suddenly flares up during COVID-19.'
'Secondly, hypothyroidism was one of the factors.'
'And obesity.'

IMAGE: A funeral for a coronavirus patient on a rainy day in Mumbai, July 4, 2020. Photograph: Francis Mascarenhas/Reuters
Why are young people of 35 or less dying in Mumbai from COVID-19?
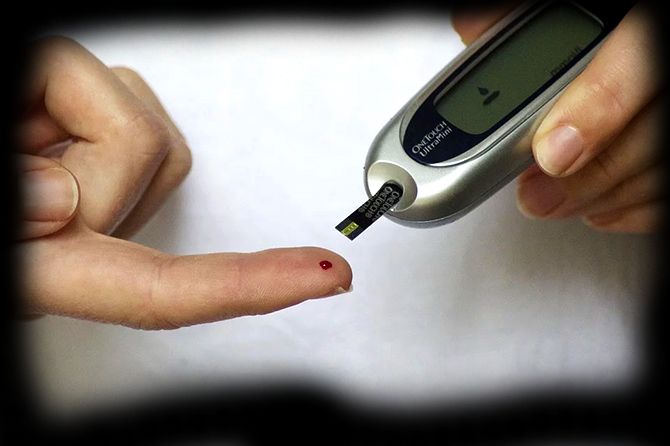
Are your elderly parents diabetic? Testing your own blood sugar could be a matter of life and death in COVID-19 times?
Since April, Dr Avinash Supe, executive director, Hinduja hospital, Khar, north west Mumbai, has been in charge of a committee appointed by the Maharashtra government to analyse COVID-19 deaths in the Mumbai urban area.
The committee of senior doctors issued reports based on their findings that are shared with city and state hospitals and the Maharashtra medical fraternity.
This retrospective analysis is invaluable because it helps reduce COVID-19 fatalities in the tough days ahead.
The committee's first report in early May discovered that most of the deaths in Mumbai in April were of males, above 50, and in patients with comorbidities like diabetes (40 per cent), hypertension or suffering from cardiac issues.
It also found that delays in diagnosing COVID-19 and reaching the hospital contributed to higher mortality.
Dr Supe, whose committee submitted a few weeks ago their second report looking at the 528 deaths that occurred in May, offers some key information on fighting COVID-19 on both a personal and societal/city level.
Work is slowly beginning on the third report, but there is a lot of data to process with the increased deaths in June.
Vaihayasi Pande Daniel/Rediff.com gives us insights into the report submitted.
Key points of a note from Dr Supe and Report II summarised here, while details are further below:
COVID-19 deaths below 40:

IMAGE: People exercise in an open gym during heavy rains in Mumbai, June 18, 2020. Photograph: Santosh Hirlekar/ANI Photo
The committee took a closer look at all patients below 40, while also spending more time analysing deaths between the ages of 41 and 50.
In May, 55 COVID-19 deaths were of younger people and 49 of them were below 40 -- a worrisome 9 per cent. That was a matter of great distress for to Dr Supe and his team.
He says: "We saw that those with non-comorbidities were also dying. That was a question of concern - that young patients were also dying.
"We started analysing these young patients and realised that they had causes, like undetected diabetes, which suddenly flares up during COVID-19. They were not on treatment and had not been diagnosed and suddenly get diagnosed during the COVID-19 diagnosis when they get admitted.
"Secondly, we also thought hypothyroidism was one of the factors.
"And obesity. It was moderate obesity."
An unexpected result of this analysis was young deaths due to hypothyroidism. Says Dr Supe: "Hypothyroidism deaths were unexplained."
Hypothyroidism is a disorder in the human body whereby the thyroid gland, located in the neck, is unable to manufacture enough of the thyroid hormone. This deficiency may interfere with heart rate, body temperature and metabolism.
The sudden young deaths lead Dr Supe and his colleagues to suggest a special regimen of care.
"We thought so these are the patients who needed monitoring. We suggested that these are the patients who should be admitted and require six-hourly (checking) of their blood sugar and pulse oximeter monitoring and you try to detect even if there is a 5 per cent drop in the oxygenation. Even when it comes down to 90 or 92 we should really put them onto high-flow nasal oxygen.
"Also give them steroids. Give them methylprednisolone. Give them dexamethasone. Give them thromboprophylaxis (drugs to prevent thrombosis or blood clotting). Give them antiviral drugs like remdesivir and also give them a tocilizumab.
"Also, do basically various kinds of proning. Proning is to put patients in prone position (on their stomachs) and ask him to undergo physiotherapy so their flooded lungs are emptied out and they breathe better."
Measures for taking care of undiagnosed diabetes:
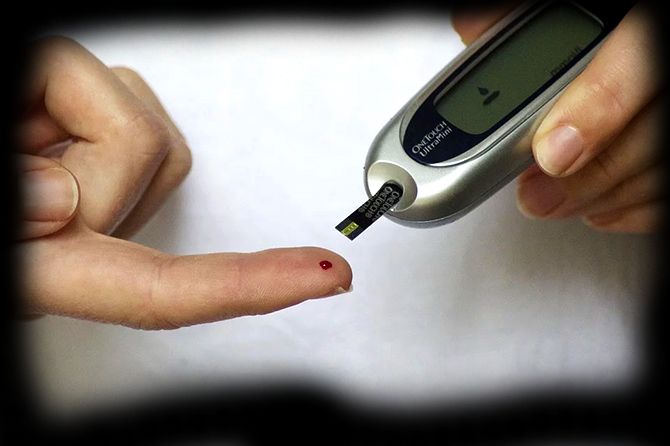
*IMAGE: One should keep a watch on blood sugar levels. Photograph: Kind courtesy Pixabay.com
The deaths of younger victims of COVID-19 suggests that everyone, sick or not, should keep a watch on their blood sugar levels. Especially those with family history or are at risk of getting diabetes for any other reason.
Dr Supe advises: "Anyone above 40 they should definitely test. With their urine they can take the home urine test.
"But I won't advise you that way unless they have some symptoms. Like say they have excessive drinking of water, excessive thirst, passing a lot of urine. They are losing a lot of weight."
"If such kinds of symptoms are there and they are passing a lot of urine, which is badly smelling, they should definitely do testing for blood sugar."
Unaccounted deaths in Maharashtra:

IMAGE: Former chief minister Devendra Fadnavis addresses a press conference in Pune, June 23, 2020. Photograph: ANI Photo
Two weeks ago, former Maharashtra chief minister Devendra Fadnavis accused the state government of concealing 950 coronavirus deaths.
Being a state committee, analysing COVID-19 deaths, details of non-COVID-19 deaths do not come to them for examination.
But Dr Supe explains the basis of Fadnavis's statement: "There is something called as a 7.1 and 7.2 ICD-10 (International Classification of Diseases) code.
"The ICMR and WHO developed a code in month (confirmed diagnosis for COVID-19) of March.
"Any patient who is COVID-19 positive and died is 7.1 and any patient who is COVID-19 suspect and who died is 7.2."
The grey area arises when, for example, a person dies of a fatal heart attack, brought on by COVID-19, but the cause of death in the death certificate is listed as cardiac arrest rather than COVID-19.
WHO guidelines, which ICMR adopted for India, specify the circumstances in which a doctor, who is filling out a death certificate, should write down the cause of death as COVID-19.
"This kind of discrepancy has occurred in many countries. Spain and US also. Same thing was seen in Mumbai also."
Subsequently, Dr Supe and his committee, he says, guided various Maharashtra urban corporations on how COVID-19 deaths are to be classified as per the WHO code.
"Corporations have responded very well and they have looked at it (the deaths) again. Last week they added some 900 deaths or something like that in Mumbai, and, overall, in India 2,000 deaths were added or something. That's the reason Mumbai death rate has gone up."
Inconsistencies over death classification is long-standing issue in India and the arrival of COVID-19 has muddied the waters further, because there can be many more mistakes in a chaotic pandemic situation.
The re-classification of death process is ongoing in Mumbai, according to Dr Supe.
"They are still sending reports. We will wait for one or two weeks, once it stabilises we will analyse."
Issues with classification of COVID-19 deaths have not happened just in Mumbai.
"It happens everywhere. Not only in Mumbai. It happened in New York. It happened in Spain. It happened in France. It happened in India. It is the way people interpret and report."
And errors in classification of COVID-19 fatalities usually emerge, as it did in Mumbai, when death audit committees swing into action.
"We said we should follow ICMR and WHO guidelines and whatever numbers are there, we accept it."
Average profile of a Mumbai COVID-19 fatality:

IMAGE: Hospital staff carry a body to a morgue in Mumbai. Photograph: PTI Photo
The second report, issued by the committee run by Dr Supe, while sifting through the higher COVID-19 deaths of May in Mumbai -- which was a reflection of "the number of cases having increased in the month of May and there was an excessive burden" -- discovered that the mortality rate of 528 deaths out of 14,521 patients (cases in the Mumbai area) was 3.63, which was lower than what was in the first report.
But the pattern of deaths were similar, says Dr Supe.
"Sixty-two per cent males and there were more patients among the elderly and there were a lot of patients who had comorbidities. Something like 60 to 75 per cent."
Outcome of the second report:
Though this committee looks at ways to reduce mortality in Mumbai, this time they took their learnings to the rest of the state as well.
"Whatever we learned from private ICUs and government doctors -- all these doctors -- we created it into guidelines and we spread it across Maharashtra.
"We took a meeting of all the civil surgeons of Maharashtra and tried to explain to them all these protocols and answered their patient-related queries. More important, what we have learned from all this, has been transmitted and disseminated (right down) to the semi-district level."
Comparison of COVID-19 caseloads in the Mumbai Metropolitan Region:
Dr Supe, who has nearly four decades of experience dealing with the city's public health, as the former dean of both the KEM and Sion hospitals (King Edward Memorial, Parel, central Mumbai, and Lokmanya Tilak Municipal General Hospital, north Mumbai), states that, even as cases multiply, totally, in the Mumbai urban area, it is apparent that cases are down in certain localities, which bodes well.
"According to me, the situation is coming in control in Mumbai in some areas. No doubt but in some areas cases are increasing -- especially in Malad*, Borivali*, Bhandup*, Dahisar*, Mulund* and Thane* it is increasing. But some areas like Dharavi*, some areas near Mankhurd*, some areas in Worli*, we are seeing less number of cases.
"But I personally feel there's more of a rise out of Mumbai, than Mumbai. Mumbai is probably coming under control. Outside Mumbai you're seeing a little rise. But we have to watch it for next two weeks and see how it is going. We are seeing more number of cases outside Thane and in Aurangabad, Nagpur."
Thane on the other hand, says Dr Supe, is showing a higher rate of increase than Mumbai.
Caseloads are increasing in Raigad district and Panvel ( a township in Raigad) but "not drastically."

IMAGE: A view of a sealed road during the total lockdown at Thane, July 2, 2020. Photograph: Anil Shinde/ANI Photo
The need for further lockdowns, area by area, functions on caseloads, says Dr Supe.
"All over, if you really see, the number of patients detected positive per ten thousand is the ratio (to go on) in a community. If the rate goes beyond 35 per 10,000 people, then you should have a very strict policy.
"If the rate is less than five per 10,000 then you can relax the social distancing kind of norms.
"Now in Mumbai we are somewhere around 8 to 10. In some areas maybe more, and in some areas maybe less.
"In those areas, where the rate is going high -- more than 35 -- should be completely locked down.
"It has now to be done locality-wise."
Time in getting to hospital and the Mumbai hospital situation:

IMAGE: A view from inside a COVID-19 care centre for critical patients in Dahisar, north west Mumbai, July 2, 2020. Photograph: Murgesh/ANI Photo
Dr Supe reports: "The median time in going to the hospital decreased in the second report from say, five days to three days. But it is still three days. But the biggest other problem was getting bed in a hospital, for serious patients, in the month of May."
He feels the situation is, since, slightly better, through June, especially in BMC (BrihanMumbai Municipal Corporation) facilities which are 90 to 95 per cent full, while it is still pretty tight in private hospitals.
The opening of the various COVID-19 field hospitals has increased quarantine areas and capacity across the city.
"If you really see now, most of our Mumbai hospitals have more beds than active patients. I was talking in the morning to many hospitals, like Rajawadi (in Ghatkopar, north east Mumbai) has 100 beds and they have 80 t0 90 COVID-19 patients. Ten to 12 patient beds are free."
Dr Supe acknowledges the need for more supportive home care for symptomatic but not serious COVID-19 afflicted, which the presently available homecare packages don't really provide.
"With our second report we had given a very classic chart and we had said use a new score - it's a British-US score and we modified it for India - and we say that any patient needs to be segregated as per this score."
The disease tosses up a range of patients -- mild patients, severe patients and critical ICU patients.
As per this score each type of patient, depending on his set of symptoms, should be headed to a different place.
"Somebody should go to a quarantine centre (CCC or COVID care centre), somebody should go to DCHC (dedicated COVID health centre), somebody should go to DCH (dedicated COVID hospital) and somebody should go to an ICU."
Before the segregation, he says, admission was being sought randomly and "there was so much of panic, people were going to whatever place which was next to them."
He feels it is now more organised and in Mumbai, in all 24 wards, it being handled at the ward level at a control centre.
Similarly, outside of Mumbai, every district has its own control centre.
There are ward meetings where representatives from all hospitals meet.
But bed capacity in any hospital is a function of staff too.
Even if physical beds exist, bed capacity comes down if there are not enough employees to man them, be they nurses, doctors or ancillary staff.
Fewer suburban trains connecting Mumbai with Virar, Palghar and Badlapur and other outlying areas, in May, caused a severe shortfall in hospital staff in Mumbai.
In June and July the problem is slightly different: "There is a lot of staff getting affected by corona. So, they are going into quarantine. The number of operational beds are less than the actual beds. Say 10 nurses in your hospital get sick so automatically you will find that 20 or 30 nurses go into quarantine and automatically your capacity comes down by three shifts and by 20 to 30 beds. That is happening in many hospitals."
Learnings from other states on reducing fatalities:
The Maharashtra committee of doctors working to reduce mortalities don't just confer among themselves but seek wider knowledge.
"We talk to Kerala, we talk to other states, we talk to all those experts around India and see what they have learnt. We consult the analysts and all that."
From Kerala they have received a bunch of tips on how to isolate people and "what are the various policies (Kerala) does and what are the various kind of rotation protocols they do."
This knowledge is being applied in Maharashtra.
Chances of survival for those with long-standing issues of diabetes:
How will severe diabetics, who have been suffering the disease for many years, be affected, if they catch COVID-19? Is surviving COVID-19 difficult if you have diabetes?
"No you can, of course. People are coming out of this.
The point is you should be in time. If you have symptoms and suspicion of this (disease) immediately go to the hospital.
If you start remdesivir within 48 hours, start oxygen quickly, start steroids in time, then the results are good.
"I have seen 90 and 80 year olds, having all comorbidities also returning home ,
"It's a question of timing, the right kind of medicines, oxygenation and proper monitoring. If you do that and glycemic controlling, most of the patients will come out of it."
*Malad, Dahisar and Borivali are in north west Mumbai. Bhandup and Mankhurd are in north east Mumbai. Dharavi is in north central Mumbai. Worli is in south central Mumbai. And Thane is a township north east of Mumbai.
Feature Production: Ashish Narsale/Rediff.com