Do we have enough trained oncologists and medical professionals in India to man these over 4,500 beds in the public sector?

The Centre's healthcare Budget saw a 9.78 per cent increase to Rs 99,857 crore (Rs 998.567 billion) for 2025-2026, with a 28.8 per cent rise in the allocation for Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (AB-PMJAY), which is now at Rs 9,406 crore (Rs 94.06 billion).
There was also relief for cancer patients with 36 cancer and rare disease drugs being exempted from Basic Customs Duty (BCD) and support for district hospitals to open cancer care centres.
The Department of Pharmaceuticals received a 28.82 per cent boost, with Rs 5,268.72 crore (Rs 52.68 billion) allocated.
The promotion of bulk drug parks rose from Rs 1,000 crore (Rs 10 billion) to Rs 1,460 crore (Rs 14.60 billion), while production-linked incentive schemes (PLI) saw a smaller rise from Rs 2,143 crore (Rs 21.43 billion) to Rs 2,444.9 crore (Rs 24.44 billion).
Finance Minister Nirmala Sitharaman announced plans to establish day-care cancer centres in all district hospitals within three years, with 200 centres opening in 2025-2026.
This initiative aims to significantly reduce out-of-pocket expenses for cancer patients.
According to the National Cancer Registry Programme, cancer cases are expected to rise, with an estimated 800,000 new diagnoses annually.
Experts have advocated for building capacity through a hub-and-spoke model for cancer care, with an estimated need for 10,000 to 15,000 more day-care beds and 25,000 surgical beds to serve all reported cancer patients.

Cancer treatment is set to become more affordable. Sitharaman proposed adding 36 lifesaving drugs to the list of those exempted from BCD.
Another six lifesaving medicines will now be subject to a 5 per cent concessional Customs duty.
These drugs include those for rare genetic disorders like spinal muscular atrophy in children and cancer treatments like Asciminib (leukemia), with some drugs currently priced in crores.
The Customs duty cuts will bring meaningful relief to patients. Currently, most cancer drugs face a 10 per cent BCD.
Furthermore, specific medicines supplied under Patient Assistance Programmes (PAPs) by pharmaceutical companies, including drugs for breast cancer (Ribociclib by Novartis), severe asthma (AstraZeneca's Benralizumab), and Crohn's disease or ulcerative colitis (Takeda's Vedolizumab), are now fully exempt from BCD. The finance minister proposed adding 37 more medicines and 13 new PAPs.
"By prioritising affordability and access, these initiatives not only provide critical financial relief to patients and their families but also strengthen the rare disease ecosystem in India," said Ruchi Sogarwal, director of corporate affairs at Takeda Biopharmaceuticals India.
Public health expert Dr K Srinath Reddy, meanwhile, said while the Budget had several welcome initiatives to improve healthcare delivery, the National Health Mission -- the vehicle for strengthening primary care and district hospitals -- had received only a small increase. This imbalance needed to be corrected, Dr Reddy added.
The Pradhan Mantri Ayushman Bharat Health Infrastructure Mission (PM-ABHIM) saw a 26.67 per cent increase to Rs 4,758 crore (Rs 47.58 billion), with Rs 4,200 crore (Rs 42 billion) earmarked for centrally sponsored schemes as capex.
The National Digital Health Mission (ABDM) allocation increased by a substantial 70.06 per cent to Rs 340.11 crore (Rs 3.40 billion).
The Pradhan Mantri Swasthya Suraksha Yojana (PMSSY), focused on correcting regional healthcare imbalances, saw a 10.4 per cent rise to Rs 9,940 crore (Rs 99.40 billion), while the central hospital budget grew 4.69 per cent to Rs 4,621 crore (Rs 46.21 billion).
--Sohini Das/Business Standard
Centre to Add 4,500 Cancer Daycare Beds Amid Manpower Challenges

The Centre is set to add over 4,500 cancer daycare beds in district hospitals over the next three years bringing it closer to the bed availability in the private sector.
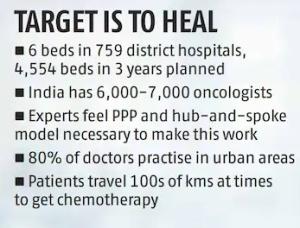
Sector experts, however, caution that the manpower to manage these beds could be a challenge, and public-private partnership (PPP) and hub-and-spoke delivery model will be developed.
Finance Minister Nirmala Sitharaman announced plans to establish daycare cancer centres in all district hospitals within three years, with 200 of them opening in 2025-2026.
A senior government official said that the plan is to have around 6 beds at every district hospital.
As of June 2024, India has around 759 district hospitals, and this works out to be 4,554 beds in three years. In 2025-2026 itself, around 1,200 daycare beds would be operational.
It can be impactful as experts feel that almost 70 per cent of cancer treatment can be delivered through the daycare mode.
At the moment, the private sector has around 6,000 cancer beds, said B S Ajaikumar, executive chairman, HealthCare Global Enterprises (HCG).
Several multi-speciality hospitals, he clarified, do not have exclusively demarcated cancer beds and much of the treatment also happens in out-patient mode.
Therefore, the private sector capacity is actually fungible and can be up to 8,000 beds at the moment. HCG, the market leader, has around 2,000 beds.
India urgently needs cancer treatment infrastructure with a crude incidence rate of 100.4 cases per 100,000 people.
Approximately one in nine people in India is expected to face a cancer diagnosis during their lifetime. An estimated 12.8 per cent increase in cancer incidence by 2025 is expected as compared to 2020.
According to the National Center for Disease Informatics and Research (ICMR-NCDIR), the projected cancer burden in India is expected to rise from 26.7 million disability adjusted life years (adjusted mortality to incidence) in 2021 to 29.8 million in 2025.
Among non-communicable diseases, cardiovascular disease contributes the most to the death rate (63.3 per cent), followed by cancer (18.1 percent).
Dr Ajaikumar, an oncologist with over 50 years of experience, said that these centres would typically need to do chemotherapies, and biopsies apart from minor procedures like blood transfusion, among others.
"They have not mentioned anything around radiology treatment, and I don't expect these daycare centres to have radiology services as well. But the daycare beds would also need highly trained manpower as cancer is not a one-size-fits-all disease," Dr Ajaikumar explained.
It is increasingly getting highly customised for each patient with genomic testing, so that the incidences of recurrence are less, he added.
This is where the challenge also lies.
Do we have enough trained oncologists and medical professionals in India to man these over 4,500 beds in the public sector? Some recent reports suggest that several states are grappling with vacant medical seats.
Odisha has more than 5,000 posts vacant for doctors in government hospitals as of December 2024.
Similarly, against the sanctioned posts of 2,689 specialist doctors, 1,559 are lying vacant in Punjab, while the corresponding figure for MBBS doctors is 1,028 out of 2,293.
In Tamil Nadu more than 5,000 posts out of the sanctioned 18,000 were lying vacant as of October.
As such, India has 1.38 million practitioners of modern medicine registered as of July converting into one medical professional per 1,263 people.
The latest Economic Survey claimed that India is on track to touch the World Health Organisation standard norm of one doctor for every 1,000 people by 2030.
The Centre plans to offer 75,000 medical seats in the next 5 years. It roughly churns out 300 oncologists a year.
The Survey also highlighted that the availability is skewed in favour of urban areas -- with urban to rural doctor density ratio being 3.8:1.
It has been estimated that 75 per cent of dispensaries and 60 per cent hospitals are in urban areas, where 80 per cent of doctors serve.
A former state government official said that in order to bridge this gap of manpower, the government is likely to plan hub-and-spoke models for delivering these services. It will also look at PPP projects.
"A city medical college can serve as the hub which will have specialist doctors and a war room of sorts that will oversee the service delivery in spokes or district hospitals. Such models have been adopted in the area of dialysis. There are post graduate medical colleges where specialist doctors and students, who are pursuing a PhD in nephrology, often man these war rooms," said the official.
PPPs will hold key to these projects as well, he added.
The patients can visit the city hospital for diagnosis and treatment plan, and the subsequent treatment can be delivered at the spokes.
"At times, patients travel 100s of kms to get their chemotherapy done and the dropout rates are thus high. Having daycare beds would reduce this burden on patients," he added.
The Centre has been running daycare cancer centres under the National Programme for Prevention and Control of NCD (NP-NCD).
At the moment, there are 372 daycare cancer centres in India under the NPNCD.
--Sohini Das/Business Standard
PMJAY allocation may not suffice, say experts

Public health experts have welcomed the increase in allocation for the Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (PMJAY) in the Union Budget 2025-2026, while raising concerns over whether these funds would be adequate to cover the expanding beneficiary base under the scheme.
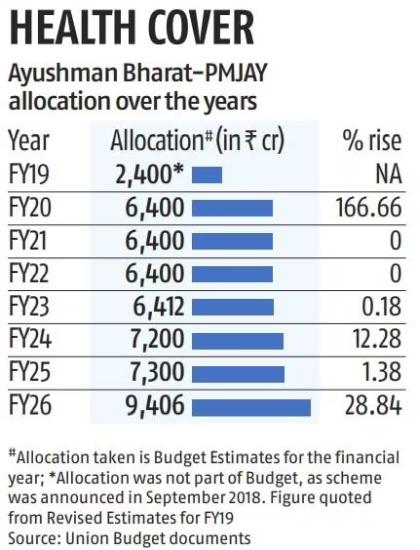
Budget estimates (BE) for the financial year (FY) 2025-2026 have put the allocation for PMJAY at Rs 9,406 crore (Rs 94.06 billion), a 28.8 per cent increase from Rs 7,300 crore (Rs 73 billion) in FY25's BE
The increase, however, comes in tandem with the inclusion of more groups and states in the scheme.
In her Budget speech on Saturday, Finance Minister Nirmala Sitharaman also announced the inclusion of around 10 million gig workers in the PMJAY in the coming years.
Commenting on the same, Indu Bhushan, former CEO for Ayushman Bharat, added that while the intention is good, there would be implementation challenges in terms of defining gig workers as they do not have a ready database.
"One can be a gig worker today and get a regular job tomorrow. Questions remain around how will the system confirm it and what process will be followed. One will have to see how these implementation challenges will be resolved," Bhushan said.
Concerns also remain if the funds are adequate to cover the expanded beneficiary base.
In 2024 alone, the scheme was expanded to cover 3.7 million ASHAs and anganwadi workers and their families for free healthcare benefits, with the year ending with the government's announcement to include around 60 million senior citizens aged 70 years and above.
This year, Odisha became the 34th state or Union Territory to join PMJAY, adding approximately 6.78 million more families under the scheme's fold.
Terming the move as a step towards universal health coverage (UHC), health expert Dr K Srinath Reddy said that while the allocation has certainly increased, "we will have to wait and see how they are going to actually increase the pool of PMJAY, with contributions from states, as well as potentially from employers (in case of gig workers), in order to provide funding for all these new categories of people who have joined."
The PMJAY, which provides cashless and paperless benefit cover of Rs 5 lakh (Rs 500,000) per annum per family in empanelled hospitals across India has been seeing an expansion in its beneficiary base since its operationalisation in 2019.
It initially covered around 107.4 million poor and vulnerable families, comprising the bottom 40 per cent of India's population, according to the Socio Economic and Caste Census (SECC) of 2011.
The beneficiary base was later revised to 550 million individuals, or 123.4 million families in January 2022.
Currently, over 365 million Ayushman Cards have been crested till now, according to data available on the PMJAY dashboard.
Hospital claim issue takes forefront
While the hospital industry has welcomed the Centre's move to increase allocation under PMJAY, it has pointed out that sustainability of the scheme hinges on ensuring adequate reimbursement rates and timely payments to hospitals.
"We support the poor people that have been able to avail treatment under Ayushman Bharat, but the delay in reimbursement payments have left various empanelled hospitals with operating losses," said an administrator for a Delhi-based hospital empanelled in PMJAY.
Several private hospital associations have, in the past, complained of lower rates and delays in reimbursement related to procedures performed under the scheme.
Just last month, the Haryana state chapter of the Indian Medical Association had called for suspension of all treatment under PMJAY in the state's empanelled private hospitals, over the issue of reimbursement payments worth Rs 400 crore (Rs 4 billion) pending with the state government.
The Private Hospital and Nursing Home Association in Punjab had announced a similar suspension treatment under the scheme last year, over unresolved payments worth Rs 600 crore (Rs 6 billion) pending for six months.
--Sanket Koul/Business Standard
Feature Presentation: Rajesh Alva/Rediff.com












 © 2025
© 2025