How can we protect ourselves against superbugs?
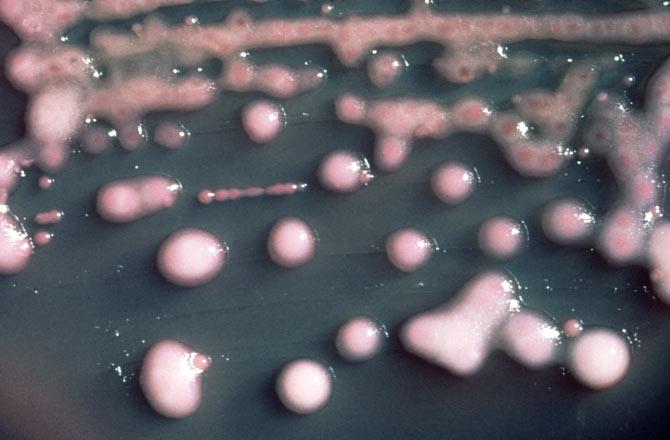
Photograph: Kind courtesy Centre for Disease Control and Prevention/Wikimedia Commons
Last week, a woman from Nevada, United States, died of a superbug infection that was resistant to all antibiotics.
In June 2016, the patient had travelled to India for treatment, which is where she is believed to have contracted the infection.
This is particularly alarming as such infections could be disastrous for health care parameters in the country.
Monica Mahajan, associate director for internal medicine at Max Super Specialty Hospital, Saket, New Delhi, tells Manavi Kapur about the dangers over-prescription and wrong usage of antibiotics pose to such infections.
How serious is the superbug issue?
Was the patient's case a single, isolated incident?
New Delhi Metallo-beta-lactamase1 is a gene which makes bacteria resistant to a broad range of antibiotics, including penicillin, cephalosporins and other stronger antibiotics called carbapenems (antibiotics used to treat infections suspected to be caused by multidrug-resistant bacteria, mainly in the hospitalised).
As a consequence, it is difficult to treat such a patient infected with the so-called superbugs.
It has two major consequences -- increased morbidity (diseased) and death in these patients and spread of these bugs to other patients.
NDM-1 was first detected in 2008 from a Swedish patient of Indian origin (who had been treated in a Delhi hospital for urinary tract disease).
Subsequently, the Centre for Disease Control, (Atlanta) described isolates (culture of microorganisms isolated for study) from patients who had recently travelled or received medical care in India.
Similar case reports were also noted after travel to Pakistan.
There were other cases in Canada (British Columbia, Alberta, Quebec) of patients who had never travelled to the Indian subcontinent. (That resulted) in a hue and cry over naming the bug after New Delhi.
Rather than naming it after the plasmid mechanism (by a small DNA molecule within a cell) mechanism by which the bacteria became resistant.
The latter would have a more scientific rationale rather than the blame game its name entailed.
Many countries including the US, UK, Canada, Japan reported cases.
In fact, NDM-1 isolates of bacteria were detected in seepage and water samples in Delhi in 2010.

In cases where a patient develops an antibiotic-resistant infection, what are the alternatives available?
The problem of superbugs is assuming bigger proportions due to two reasons.
(Firstly) with international travel and medical tourism, the bug may be spreading beyond boundaries.
Second, treating these patients is difficult.
Antibiotics, like colistin/polymyxins or tigecycline, may or may not work.
There is high mortality in these patients.
Adding to this problem is the issue that routine labs cannot test for NDM-1 resistance.
It is suspected the culture is resistant to carbapenem antibiotics.
There is no clinical parameter for identifying these patients by mere physical examination.
The worst nightmare is that there are no major antibiotic drugs in the pipeline to counter these superbugs.
On a policy level, how can the problem of over-prescription be contained?
The reason why India got into this controversial situation is that there is no regulated use of antibiotics in our country.
Any doctor or pharmacist can prescribe an antibiotic even for viral infections where no antibiotic is required.
The 'restricted antibiotic policy' to avoid unnecessary use of higher end antibiotics only exists on paper.
Most hospitals do not collect data about resistant bugs or develop an antibiogram to guide their treating physicians.
There has to be an anti-microbial stewardship programme in hospitals where the microbiologist and pharmacist monitor injudicious use of antibiotics.
What are the precautions that should be taken by doctors and patients while prescribing and using antibiotics?
Hand washing in hospitals should be the norm and part of the work culture.
Patients with resistant infections need to be isolated with strict barrier nursing.
There should be a central registry for recording resistant cases.
Cooperation rather than the blame game is needed at the international level to find solutions to this evolving problem.
At the personal level, patients should avoid self medication with antibiotics or taking incomplete courses of antibiotics to avoid developing resistance to antibiotics.
Visitors to ICUs need to be restricted in the larger interest of patients.
Visitors to ICUs also need to adhere to hand washing.







