 Leading state-run general insurer New India Assurance Company on Wednesday said it will soon launch a new premium mediclaim product as a part of its efforts to resolve the issue over the cashless health cover, which the state-run players had discontinued early July alleging inflated billing by hospitals.
Leading state-run general insurer New India Assurance Company on Wednesday said it will soon launch a new premium mediclaim product as a part of its efforts to resolve the issue over the cashless health cover, which the state-run players had discontinued early July alleging inflated billing by hospitals.
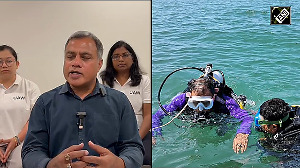
"We will shortly launch a premium product with the cashless option so that the consumer has the choice of cashless hospitalisation at premium corporate hospitals," New India Assurance Company chairman and managing director M Ramadoss said.
Ramadoss further said, "The acquisition of cost of this product will depend on the type of scheme one chooses. If one wants hospitalisation in a corporate hospital, then the premium will be higher."
The move is also aimed at bringing corporate hospitals under its fold, Ramadoss said, adding it is adding three Delhi-based leading corporate hospitals-Gangaram, Max and Medicity--to its empanelled list of hospitals for this scheme.
The move comes on the heels of the sectoral watchdog Irda recently stating that companies were free to launch premium products to bring five-star hospitals under the cashless cover scheme and that the Authority has no role in fixing prices.
"If you want to stay at Ashoka Hotel...and avail of five star facility, you need to pay more," IRDA chairman J Hari Narayan had said in the Capital earlier last month.
The IRDA Chairman's remarks came a day after the Delhi High Court asked the insurance regulator to sort out the imbroglio over the cashless facility to policyholders in major hospitals across the country.
The regulator, however, held the view that it could do nothing in this regard. "We have long moved away from the administered price regime and it is for the market forces to determine the price of their products," Narayan further said, adding there might be co-payees or higher premium products for these five-star hospitals, which the insurers should decide.
Clarifying on the PSU insurers' recent decision to discontinue cashless policies, Ramadoss said the company was never against cashless claims but wanted some clarity on the tariffs being charged by most of the hospitals empanelled, which the insurance industry felt were inflated.
Claiming that the issue has been blown out of proportion by the media, he said, "only 35 per cent of health polices are cashless ones and that just 8 per cent consumers make the claims through hospitalisation."
On whether insurers would be setting the price bracket, he shot back saying, "we cannot and do not want to do that. We are just suggesting that the hospitals come out with a tariff plan and then stick to them."
The cashless facility was discontinued at all major hospitals from July 1, as they refused to lower their rates for many of the standard procedures. Four major PSU insurers, which command 80 per cent market share of the health insurance business, demanded that hospitals should agree to the package deals if they wanted to be on the preferred network service and benefit from the cashless system.
The 18 general insurers including the four PSUs, took the extreme step as they annually bled Rs 1,500-crore (Rs 15 billion) more than what they collected as the premium from the mediclaim policies while settling claims of hospitals across the country.










 © 2025
© 2025